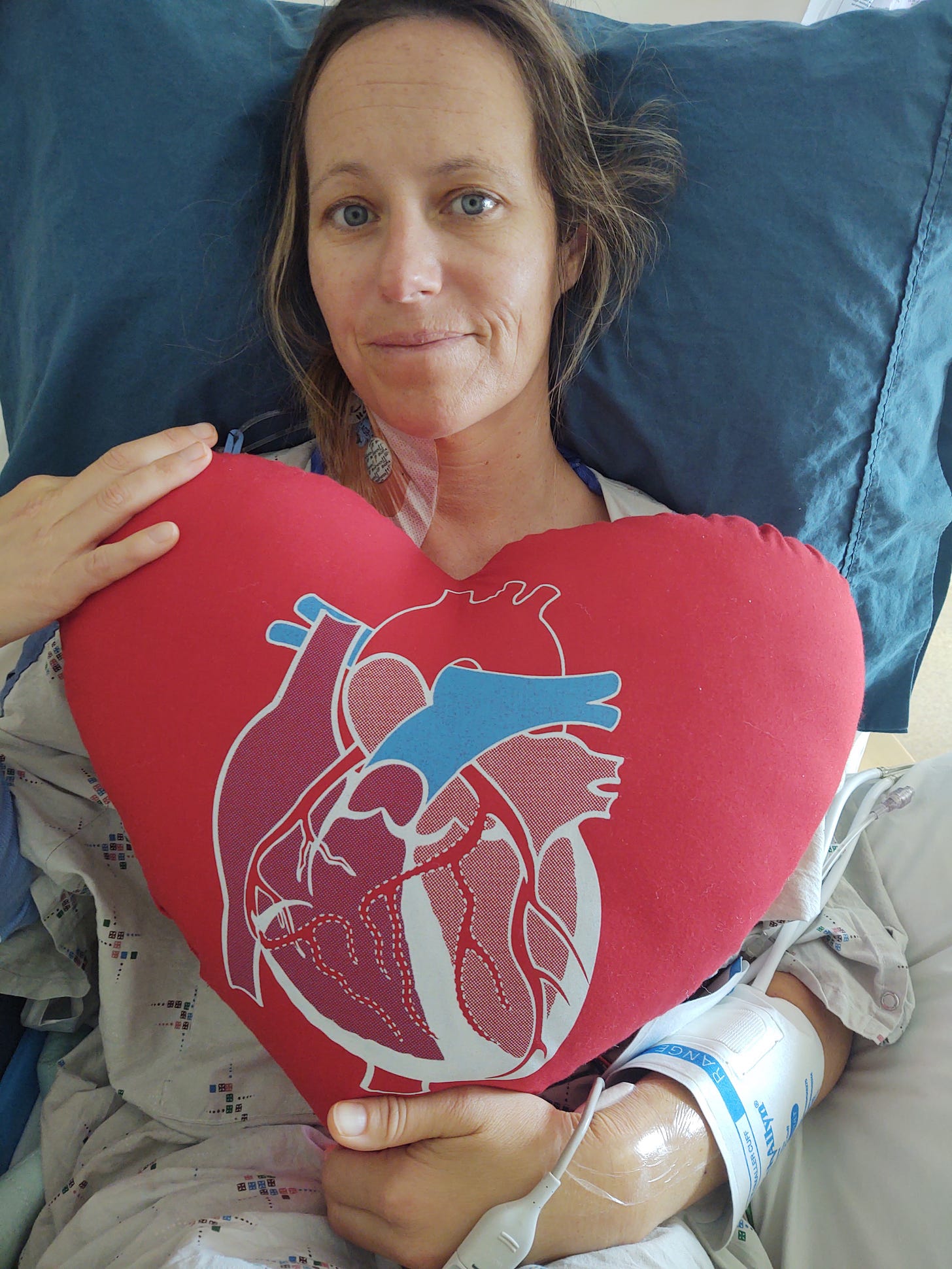
Today I am celebrating one year post open heart surgery. It truly is a new birthday for me. I have been wanting to tell this story in as much detail as I can recall. I want to have record of it for myself and my family. But I also want to answer some of the many questions you may have about when and why and how. I was honored to be included by Manduka this past month in a campaign they were doing on “Inspire the Practice.” For those of you that are not aware, Manduka (a yoga mat company) was one of my corporate clients for many years. I worked in office for them as a yoga instructor. The people of Manduka are truly my family. They helped me start opening up about my journey this past year through the campaign. But I felt there was still a part of my story unsaid. I feel lucky to be in good health today, one year later. This story is filled with fear and sorrow, but also strength, patience, resilience, trust, and love.
I have always taken good care of myself. Like most people I have gone through waves of really feeling excellent, and then suffering from lulls usually from over indulging in life. For the past fifteen years I had also had waves of not feeling “right.” The feeling would come and go. In the past I had tried to find out what might be going on with me, but never landed in the hands of the right doctor to work with. I had been feeling more fatigued then normal since giving birth to Miller in 2018. In the fall of 2021 I finally got myself to find a doctors office that I liked. Someone who would do some blood work for me to investigate the fatigue and migraines I had been experiencing since Miller was born. Most people I spoke with blamed it on having a small child, but deep down on my gut I could tell it was something more. For all the years I had experienced bouts of “not feeling right” it was finally time to dig deeper. My new practitioner saw some clues in my blood work. She told me to take some supplements and come back in 6 weeks to do more testing. Well that second round didn’t happen because their whole office was practically shut down due to COVID. In mid December we went on fun ski weekend in Mammoth. My husband Mike had a cold all weekend but I felt great. The last day while driving home in the car back to Reno I asked myself the question, “Am I finally getting this cold he’s had the past 5 days? Darn-it!” I had been feeling invincible.
I got the cold and then some. It was a week before Christmas and I assumed it would be gone by the holidays. We considered not having family come, but after multiple negative COVID tests they decided they wanted to come anyways. I was so worried to pass along this cold, for me it wasn’t it quick five days, it wouldn’t go away and only kept getting worse. By January I went in to see my practitioner and they gave me steroids for what was now a pretty bad case of bronchitis. They told me to go to urgent care if it doesn’t go away so I could get a chest x-ray. A month into this sickness I went to urgent care. Yes I had bronchitis, but still no to pneumonia. And now yes to COVID. Mike had tested positive at home. This was the main reason I went in to the doctor’s office. I was worried about COVID on top of my month long cold. Well COVID came and went, and yes it was worse for me being sick already, but I survived fine. And now I was left with bronchitis still. In February I had started to have weird symptoms that were not normal for a cold. Confusion, problems with sight, my brain was not feeling right. Night sweats had started before COVID but had gone away for a while and now we’re back and concerning. Many people blamed it on Long COVID but I was not convinced.
Fast forward to early March… Although not feeling one hundred percent, I felt okay enough to take my daughter Miller to Manhattan Beach for a long weekend. While there I pushed through, but underneath it all I could tell something was really wrong and just wanted to get back home. My whole trip I was telling all my friends I just don’t feel right. I was having terrible night sweats. I couldn’t think straight. I felt like I couldn’t breathe. I came home and finally got that second round of blood work I had wanted a day later. We did deeper dive and some more rare testing. And four days after getting back home I fell acutely ill with a severe fever. I could barely get out of bed so I went to the ER. Even then I was trying to push thru it, but in the recent days two different people told me stories of how someone they new had gotten deadly sick and hadn’t known it. It was time to get answers. I went to the hospital thinking I’d be back with the right meds finally. I was admitted. And there started the journey to this whole thing that I finally had a name for.
Thank goodness my first ER doctor wanted to figure things out. My blood work from a few days previous had come back that I had active Epstein-Barr. I also had Sepsis. But he also thought there was something else beneath it all so he kept digging and many, many different tests later he found bacterial infection that landed on my aortic valve and created a mass. I had Bacterial Endocarditis on top of the Epstein-Barr. The Endocarditis was much more serious and we needed to focus on that first. Talk about adding insult to injury. The doctors felt my blood work showed I might have another factor that we had not discovered yet. Maybe that was the thing that has been making me feel fatigued over the years. But that was going to have to wait until I dealt with the endocarditis.
This is where everything is a little blurry in my mind. And you can probably tell by now I wasn’t an English major so bare with my writing skills…
That first hospital stay was a handful of days. I was tested for everything. When your body is sick and weak, whatever may be in a dormant state may it be bacterial strains, and or viruses may take this as an opportunity to become active again. We needed to act right away. We decided to go the conservative route and try antibiotics for four weeks hoping that would take care of the bacterial infection and would help me avoid surgery to have it removed. My infection was caused by the viridian streptococci bacteria. Commonly found in the mouth but also there upper respiratory tract. We still aren’t sure why I wasn’t able to fight off this common bacteria. I had my midline set in my upper right arm to take the daily antibiotic injections and was sent home.
We needed help at home with Miller and family and friends stepped in (thank you). A handful of days after being home my mom was set to come help with Miller. The day she came in I had been feeling some stomach pains and also had been having a hard time with my antibiotic injections. Doctors instructed me to go back to the ER to make sure things were going smooth. My mom arrived in the afternoon, and literally ten minutes later we left to figure things out at the ER. Unfortunately and unexpectedly I was admitted again. I had formed a blood clot in my arm so the midline had to come out. I also had minor Gallstones (go figure)…but more importantly, things had gotten worse with the infection, and after many more tests later it was determined I was going to need surgery in the next few days. My body was shutting down. My life depended on it. Things kind of get even more blurry from here on out. Many tests to figure out many different things that were going on with me or not going on with me. Many days of sitting and waiting, sleepless nights. More tests, more meds. And finally the decision was made to stay in Reno for the surgery which was set for March 31st.
We had debated about going elsewhere for the surgery. Naturally, I wanted the absolute best doctor to work on me. Friends had helped us get connected with a doctor in San Francisco who was doing surgeries similar to what I needed and with the potential to be less invasive (not open heart). Ultimately we decided to stay with the CT surgeon we had been working with here, Dr. Knackstedt. After talking to him and seeing his perspective on my situation I felt very comfortable with him moving forward. He seemed like a gentle giant. He reminded me of one of my best childhood friends, and that gave me comfort. He set my mind at ease but he also scared me by telling me all the percentage points of what could go wrong including death. I was too tired and too sick to go elsewhere at this point. It was time to move forward.
If you’ve been following my story you know that I had many complications along the way. Problems with my medicines, midlines, IV lines, allergic reactions, etc. Lots of fevers. Hundreds of tests of all kinds. And a lot of unknowns. That’s the stuff I’ve kind of blurred together… it’s less important to detail all of that so I’ll continue on with my Cliff Notes version of what I have been through.
After that second ER visit I never left the hospital before my surgery as they kept me that whole week preparing me for the day of surgery. I would need to stay at least five days after surgery which was a long time to be away from my family. The hospital made some exceptions and let Miller and my mom come to visit me the day before surgery which was definitely a boost in my mind for positive thoughts going forward. Did I fear it may be the last time I would see my family? Yes. There was a chance of death from the procedure. A 3% chance, plus other complications. I was scared.
March 31st, 2022 was surgery day. I had to do a TEE (echocardiogram) before my surgery where they went down my throat to take a look at just what they were going to be operating on. After that was completed I was off to the OR. I remember waiting to go in. I can remember meeting the team in the surgical room of at least 15 people moving about getting things ready. It was a bigger room then I expected. It was very cold. They played loud music, I think 80s. It was longer than I imagined before I was out. Next thing I remember was waking up to the tube down my throat that needed to be left in for a few hours. I had tubes coming out of my abdomen as well, draining fluid from my body. I had been on the heart and lung machine for an hour and a half during surgery. The total surgery three hours I believe. Recovery was tough the first few days. But I had good nurses, David was my favorite. Thank you David! He took good care of me and it wasn’t pretty! There was construction below my room which made rest hard to come by. (Why a hospital would allow that still boggles my mind) The physical pain was very real. But daily I saw improvements. I needed lasix diuretics to pull the excess 25 pounds of fluid off of me from surgery. Mike said I was almost unrecognizable for a brief time! I also needed to have multiple blood transfusions. My body had been so depleted. I was slowly getting better. Five days later they discharged me, believing that with all the noise at the hospital I would be better to recover at home. My good friend Tina recalls I called her crying saying they gave me a Xanax and a tea from Starbucks and kicked me out of the hospital! Not true entirely, although my medications would make me think so. I could barely move on my own. Going home was scary.
One thing we didn’t do before I left the hospital is go back to my original antibiotic medicine that would be administered through my new midline on the non blood clot arm for the next 4 weeks. I had switched to penicillin while I was at the hospital. We were going back to Ceftriaxone. I had been on it before so nobody thought twice about it. The first time I received the medicine at home the following day I had a terrible reaction to it. It was the only time I went back to the ER via ambulance. Mike said the men in the house from the fire department were the best looking guys in Reno…ha ha. Even one of the guys who had been on the TV show The Bachelorette was there. I was so out of it I pretty much missed it all. I don’t remember much of that ER visit. The Doctors had told Mike I was VERY sick this time and they were not sure why, and he needed to be prepared. Landing back in the ER bought me a few more days at the hospital, I can’t even remember how many at this point. They switched me back to penicillin and I would stay on that until I was done with my antibiotics. I would have to wear a Fanny pack that held the meds in a compression ball that continuously infused me…its a good thing I liked fanny packs!
When I finally did make it back home it was a slow road. I know there were multiple more ER trips. My last ER stay was at the end of April when my sister was in town helping. To all the people who were able to make it out and help me thank you so much. You will forever be woven into my story and I couldn’t have done it without you. My girlfriend Shannon was there at the beginning I can’t even believe how much I have improved since she had been helping me. I couldn’t even sit up in a chair by myself at that point… When my sister was in town I laid on the ground for the first time, it had already been a month past my surgery. Laying on the ground was so difficult. I was only there for about a minute and I was in pain for a couple days because of it. Tina was the master of making us meals! But more than anything, everybody helped so much with Miller. And Miller feels so connected to all of you, so thank you very much for taking care of our family. At 12 weeks post-op I was still unable to pick Miller up. Just to give you an idea of how long my recovery was.
Back to my last ER trip(s)…As I was nearing the end of my antibiotics at the end of April my veins were just so tired of being poked. I went into the ER to have it looked at and they kept me for I believe three nights. I needed to switch my midline to a new location. I was running out of veins that were able to handle the constant injection. The last night I was there was because there were no doctors or nurses who could set my new midline and I was furious to be just sitting in the hospital waiting. It was the first time I had really freaked out at the hospital and I was losing my mind. I had been on an IV constantly now for over seven weeks. I was going home the next day no matter what I told them. I woke up to the same dilemma. Nobody who could set my midline… Does the hospital not operate over the weekend? My doctor for that stay allowed me to leave, but not what she wanted me to do. I left with a regular IV in my arm (it was unheard of) as long as I went back to the ER the next day to have the new midline set. They let me do it because they were concerned for my mental health. It seems like a lot of work to go back to the ER, but to me it was important to be home with Miller. The next morning we went in at 7am. They had a horrible time finding a place to set the midline. The first nurse I saw put so much fluid in my arm missing my vein she gave me Phlebitis. She was super cocky that she was doing things right… Phlebitis is when your arm is completely swollen, doubling in size. It takes about 8 weeks to go back to normal. Mine lasted about that, and my bicep was sore for about 3 months after. They brought in a ultrasound machine and a specialist and found a vein in the same arm they had missed in. I only had 3 days of antibiotics left, what could go wrong? Well I was back in the ER the very next day because of the phlebitis. I was so worn out from all of these different ER visits I’m sure I missed a few in my story here. I had two more days with the antibiotics and we went home.
Turns out we made it almost to the end. Thanks to all my nurse friends for helping me in the final hours of my midline. I refused to go back to the ER again. If I went I may get admitted and I was so over it. We had decided to end my antibiotics 12 hours early. In the long run that doesn’t seem like a lot but we were afraid that it would affect my recovery and the ridding of the bacterial infection. My arm was so swollen from my last ER visit. Eventually my arm was so swollen it pushed anything that was going into my vein right back out. We didn’t even know if I was getting the medicine anymore. That day when we decided to pull the IV out at home which seems a little risky I immediately started feeling better. Don’t worry we did consult the pharmacist before we did it. I was finally done with antibiotics I had been on them for so long.
Turns out ending the antibiotics early did not affect my recovery. Doctors visits and follow ups after have showed that I am doing great. There is no more bacterial infection. Epstein Barr has run it’s course. And no more ER visits. I had a home nurse that came to check on me a couple times a week. It cut the trips to the doctor in half. I had a new healed heart that would require a lifetime of blood thinners. But I was alive! In mid-May 2022 I was accepted to the cardiac rehab program. I participated in this program three days a week for two hours a day for 12 weeks. It was a group class, one hour of education and one hour of workout. This program was vital in my recovery. Working out with nurses by my side was the confidence booster I needed to push my heart and get it thumping again!
I can’t tell you how much stronger I have gotten in this past year. I might be in better shape now than I was before I got sick. Once my cardiac rehab program finished I decided to keep up the momentum by getting a trainer and working out with her a couple days a week. The past six months, she has kept me on track. Its the best thing I have done for myself in years. I was told that the full recovery was about a year. And I would say that’s close to correct. Lately I have been feeling more like myself. There are still “leftovers” from being sick, but I don’t feel like I am sick anymore. I am taking way better care of myself these days. I am finally taking a deeper dive into why I may not have been able to fight off this infection and finally feeling closer to answers. Not that I need to know how it happened, but more so to stay healthy moving forward.
I will leave you with some stats of the sick months. 30 total days in hospital, 9 trips to ER, 47 days of IV therapy, 15 post-op out-patient visits, 36 days of physical therapy. This last one is crazy: weight going in to surgery 120lbs, weight right after surgery 140lbs, weight 3 weeks post-op 110 lbs, weight 12 weeks post-op 115lbs. And I am happy where I am now and have stopped checking!
Thank you for following my journey. It is very healing for me to share. I have wanted to document this experience. I hope this can help shed some light on my illness and the recovery. But also help anyone out there who may be going through something similar.
Today I am busy getting back to life. I have started to share my yoga teachings again slowly on Youtube, and hopefully that will translate into something more. I decided to start this blog, which I have though about doing for years. I am taking care of myself with healthy diet, exercise, yoga, meditation, acupuncture, massage, saunas, cold showers and so much more. And I plan to just enjoy each day. We never truly know when those days may come to a screeching halt. Hopefully I bought myself many more years.
Love, Anne







Wow Anne. I knew you had been one one heck of a journey but I had no idea just how much of a ride you’ve been on. Thank you so much for sharing so vulnerably and being willing to be so open. I think it can help so many people not only who might be experiencing something similar or health related but also serve as a beautiful reminder of just how incredible and resilient our human bodies are. You are amazing. You are wonderful. You are such a bright light. And I’m honored to know you. Wishing you continued health on your journey. And sending you a lot of love! 💗
Anne—
Thank you for sharing. What an unbelievable journey you have been on! I am so happy to hear you are on the other side. It is so tough to go through all this with a small child! I hope you continue to heal and sending lots of love to you and your family!